St. Luke’s telehealth expands, innovates during COVID era

It is said that necessity is the mother of invention.
And while St. Luke’s hasn’t historically waited around for necessity to visit, it’s fair to say that COVID-19 has accelerated the rate at which some programs and initiatives have developed.
With COVID-19 precautions limiting face-to-face interactions, telehealth has become a vital extension of St. Luke’s clinics and hospitals.
Video visits with providers have increased by a massive amount this year. About 0.1% of clinic visits were done via telehealth prior to March. Now, that number is 12 to 20%, with nearly 200,000 completed the last 10 months.

A program that St. Luke’s adopted in 2017 – remote patient monitoring (RPM) – has seen similar growth.
Prior to May, the program had been used for about 350 patients; in the past seven months, it has been used for 640 patients, nearly double the use of the previous three years.
“We were forced to act quickly, but it has shown us how telehealth is a useful service that will stick around,” said Krista Stadler, senior director of telehealth for St. Luke’s Health System.
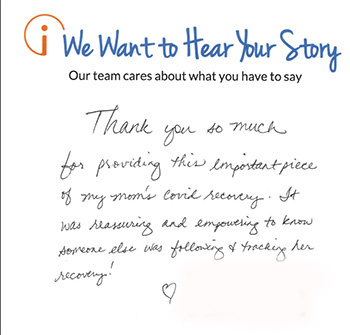
Remote patient management was quickly deployed early in the pandemic and is an integral part of recovery for COVID patients recovering at home following a hospitalization. RPM uses devices to connect patients with doctors and nurses at the Virtual Care Center in Boise. It allows for consistent supervision, and for anytime access for patients.
Once qualified patients are on the road to recovery, they are sent home with a kit that includes a blood pressure cuff, scale, pulse oximeter and a tablet. The tablet allows the patient to be in the comfort of home while still communicating with providers, who are able to monitor changes in patients’ conditions, symptoms and emotional needs.
“We were very fortunate at St. Luke’s, that our leadership, saw this could be a program that would transform our clinical model,” Stadler said. “That foundation paid tenfold when suddenly we were forced to change how we practiced.”

The kits connect to cellular networks, so even patients in rural areas or without WiFi access can use them.
“We’ve had a 104-year-old use it,” said Jason Blomquist, St. Luke’s director of telehealth and virtual care services.
Given the nature of COVID-19 and the resource factors and complications involved in treating those who have fallen ill as the result of exposure to the novel coronavirus, digital care approaches, when appropriate, are proving highly effective. And there are the mental and emotional elements to consider as well.
“You cannot underestimate” the healing environment of being in your own bed, Stadler notes.
The program has been expanded to include other patients in Boise, Meridian, Nampa and Magic Valley. Patients who often are good candidates for inclusion in the program include those with chronic obstructive pulmonary disease (COPD), congestive heart failure, pneumonia, sepsis and Type 2 diabetes.
In early December, 175 patients were being monitored, with capacity increasing to support 300 to 600 participants in January and plans to accommodate as many as 1,500 at once.
St. Luke’s Virtual Care Center is abuzz with activity as nurses, doctors and specialists monitor and speak with patient participants in the program and other digital services. Launched in 2018, the center is open 24 hours a day, seven days a week, 365 days a year. About 50 providers are there on any given day, with plans to add about 20 more very soon.
In March, as COVID-19 swept across the region, the center provided eight telehealth programs. By the end of January, there will be 29. Hospitals across the region who are linked to the center can get immediate support from specialists not necessarily available to them in their physical locations.
The pandemic has underscored what St. Luke’s leaders realized regarding the value of appropriate, well-planned online health services. Patients at clinics and hospitals can connect with specialists at the Virtual Care Center via video. Specialties include urology, neurology, sleep medicine, cardiology, psychiatry and more.
In less than a year, 300 additional hospital rooms have been wired for virtual care, and more than 73,000 virtual connections have been made with hospitalized patients since March 1.
“COVID is a part of that, but it’s also this realization that we can actually do this, that it makes a lot of sense,” Stadler said.
“The ability to do this work in record time was not accomplished by one team, but rather by our entire St. Luke’s family stepping up and leaning in,” Stadler added.
“We have come together like never before.”
About The Author

Dave Southorn works in the Communications and Marketing department at St. Luke's.

