Patients Credit St. Luke’s Physicians, Technology for Nearly Painless Surgery, Quicker Recovery

St. Luke’s added the da Vinci® Xi, the latest version of a robotic surgery system, to its technology collection this past fall. Patients and physicians say they are enthusiastic about the results they’re seeing with minimally invasive technology, new and old.
Vaughn Olson, an aircraft demonstration pilot in Boise and former U.S. Marine, remembers the agonizing pain of having his appendix removed through traditional surgery and the long recovery while he was in high school.
“It felt like I was a pie that someone cut apart and stuck back together,” he said. “It hurt like crazy.”
In comparison, he said a more complicated surgery in February to remove a cancerous prostate “was nothing” due to the skill of St. Luke’s oncology surgeon Dr. Stephen Brassell and St. Luke’s new da Vinci Xi Surgical System – minimally invasive robotic technology.
“I had six small incisions,” Olson said. “Basically, I had no pain afterward. I was out of the hospital in two days.”
About four months later, Olson says he’s completely cancer free and almost back to normal.
“He got it early,” Olson said. “He’s so confident. His confidence paid off. He’s a rock star. Everything he said was true.”

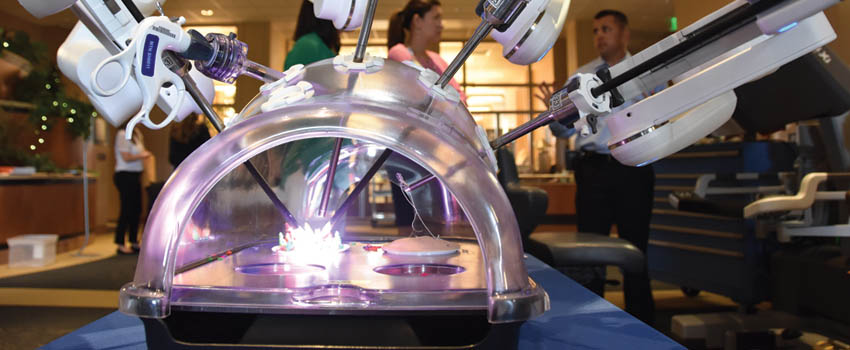
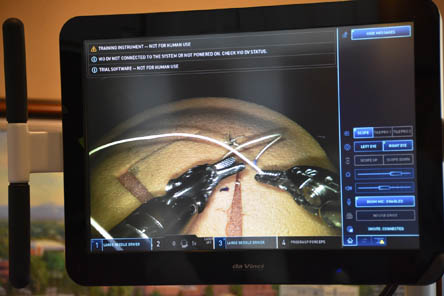
St. Luke’s Boise now offers the latest da Vinci, the Xi – one of about 215 worldwide and the only one in Idaho. The Xi instrumentation translates physicians’ motions into smaller, more precise movements with far more dexterity and control than human hands.
Four robotic arms hold small instruments to hold and cut, an endoscope with a camera and a light, which can be moved to any of the arms, allowing surgeons to see into different areas of the body when operating without moving the patient or the robot.
For patients, the benefits of combining skillful surgeons with the latest minimally invasive technology of da Vinci are less pain, blood loss and risk of infection, fewer complications, shorter hospital stays, and faster recovery.
Every day, St. Luke’s surgeons use da Vinci Surgical Systems for a variety of operations, including prostate removal, gynecologic surgeries like hysterectomies, adult and pediatric urological surgeries, hernia and gallbladder, and removal of various cancers.
This isn’t just for one field, one specialty,” said Dr. Kara Saperston, a pediatric urology physician who uses the da Vinci Si when appropriate with younger patients.
Saperston said using the da Vinci Surgical System means a faster return to school for kids and to work for parents. Parents and adults considering robotic surgery should discuss it with their doctor to decide if the daVinci is right for them.
In April 2015, Saperston operated with the da Vinci on Joy Fenske, 7, of Middleton to correct vesicoureteral reflux (VUR), a condition in which urine flows back into the tubes (ureters) from the bladder toward the kidneys, causing urinary tract infections and other problems. Left untreated, the condition can cause repeated urinary tract infections and long-term illnesses such as kidney damage, diabetes, and high blood pressure.
“I couldn’t be happier,” said Danielle Fenske, Joy’s mother. “She came home, and I had to stop her from being too active. We caught her running outside, down a hill. I was so pleased I had to hold her back.”
Joy is the third Fenske child to be treated for VUR, a hereditary condition for her family. However, the robotic surgery wasn’t available for her older sisters, Grace, 13, and Eileen, 11. Grace had open surgery for VUR when she was 8. Eileen had a lower grade of VUR at age 9 and was treated with a less invasive procedure, which was still painful with a longer recovery period, Danielle Fenske said.

“With the full open, there’s a ton of blood, and that is hard to deal with in a kid,” Danielle Fenske said. “For a kid, that’s scary to see. There are tons of bladder spasms. Using the bathroom is hard to do because there is lots of burning and stinging. The other difficulty is the incision pain. To this day, Grace is still sensitive on her incision.”
Danielle attributes Joy’s good result to Dr. Saperston’s skills as well as the technology. And she praises the doctor’s compassion and caring, saying Dr. Saperston stayed in touch – even texting to check in late at night.
“If I had to choose again, I would choose robotic over the less invasive procedure or open surgery because of the stinging and burning involved,” Danielle said. “She is such an amazing surgeon. St. Luke’s Pediatrics is so amazing.”

About The Author

Sandra Forester works in the Communications and Marketing department at St. Luke's.


